Why Kentucky needs a
Health Data Utility with claims data
A Health Data Utility integrates electronic health data from across care and service settings to support treatment, care coordination, quality improvement, and community and public health initiatives. When the utility includes insurance claims data, it offers a more complete picture of where and how health care dollars are being spent- enabling smarter policymaking, resource allocation, and accountability.
A Health Data Utility & MOAB Findings & Recommendations:
The state’s Medicaid Oversight and Advisory Board (MOAB) was convened amid growing concern that Kentucky Medicaid is financially unsustainable, lacks transparency, and is difficult for policymakers to meaningfully oversee. Over multiple meetings, the Board concluded that legislators do not have timely, reliable access to the data needed to independently evaluate spending, performance, access, or outcomes.
The Board’s findings underscore that Kentucky cannot effectively manage Medicaid—or broader health system challenges—without better information and governance. Legislative oversight is currently limited by fragmented data systems and insufficient analytic capacity. Establishing a statewide Health Data Utility would directly address these gaps by creating a centralized, independent source of health data that supports legislative oversight, transparency, and accountability.
Who benefits from claims data and how?
-
Insights from claims data will enable research and data-driven policies that could lead to higher quality of care for Kentuckians. Claims data would improve price transparency which could reduce unnecessary expenses for care that increase out-of-pocket costs for consumers.
Learn more. (The APCD showcase shares how other states have benefited from claims data collection through All-Payer Claims Databases.)
-
Claims data can help providers and hospitals better understand patient populations, identify trends, and make more informed decisions about care delivery. By providing comprehensive data on health care utilization and costs, claims data can help health systems operate more efficiently, provide higher-quality care, and ultimately improve the health and well-being of their patients and communities.
Learn more. (The APCD showcase shares how other states have benefited from claims data collection through All-Payer Claims Databases.)
-
Claims data would give state and local policymakers the full picture of the complex landscape of health care spending. By showing where the costs are coming from and where the burden is falling – claims data can inform research and policies that save money, increase access to care, and improve health outcomes.
Learn more. (This link shares how policymakers in other states used claims data from an All-Payer Claims Database.)
-
Claims data would allow employers to see the full impact of various health insurance plans- from costs to quality of care. This would assist with benefit design and planning, allowing employers to improve health outcomes while more effectively managing their healthcare expenses. It would also aid in implementing and complying with new federal fiduciary and transparency rules that require employers to pay a “fair price” for health benefits.
Learn more. (The APCD showcase shares how other states have benefited from claims data collection through All-Payer Claims Databases.)
-
Claims data would provide insurance companies with a number of benefits, including: comprehensive cost analyses; a means for identifying fraudulent activities; improved care coordination and overall quality improvement; and pricing and risk assessment.
Learn more. (The APCD showcase shares how other states have benefited from claims data collection through All-Payer Claims Databases.)
Access to claims data would be a win for Kentuckians.
It could lead to a higher quality of care and better health in Kentucky, while also identifying ways dollars can be used more efficiently… thus reducing unnecessary expenses for care that increase out-of-pocket costs for consumers.
How claims data is guiding policy in other states
These states use All-Payer Claims Databases. But a Health Data Utility in Kentucky that gathers claims data could be used in similar ways.
Claims Data Myth Busters
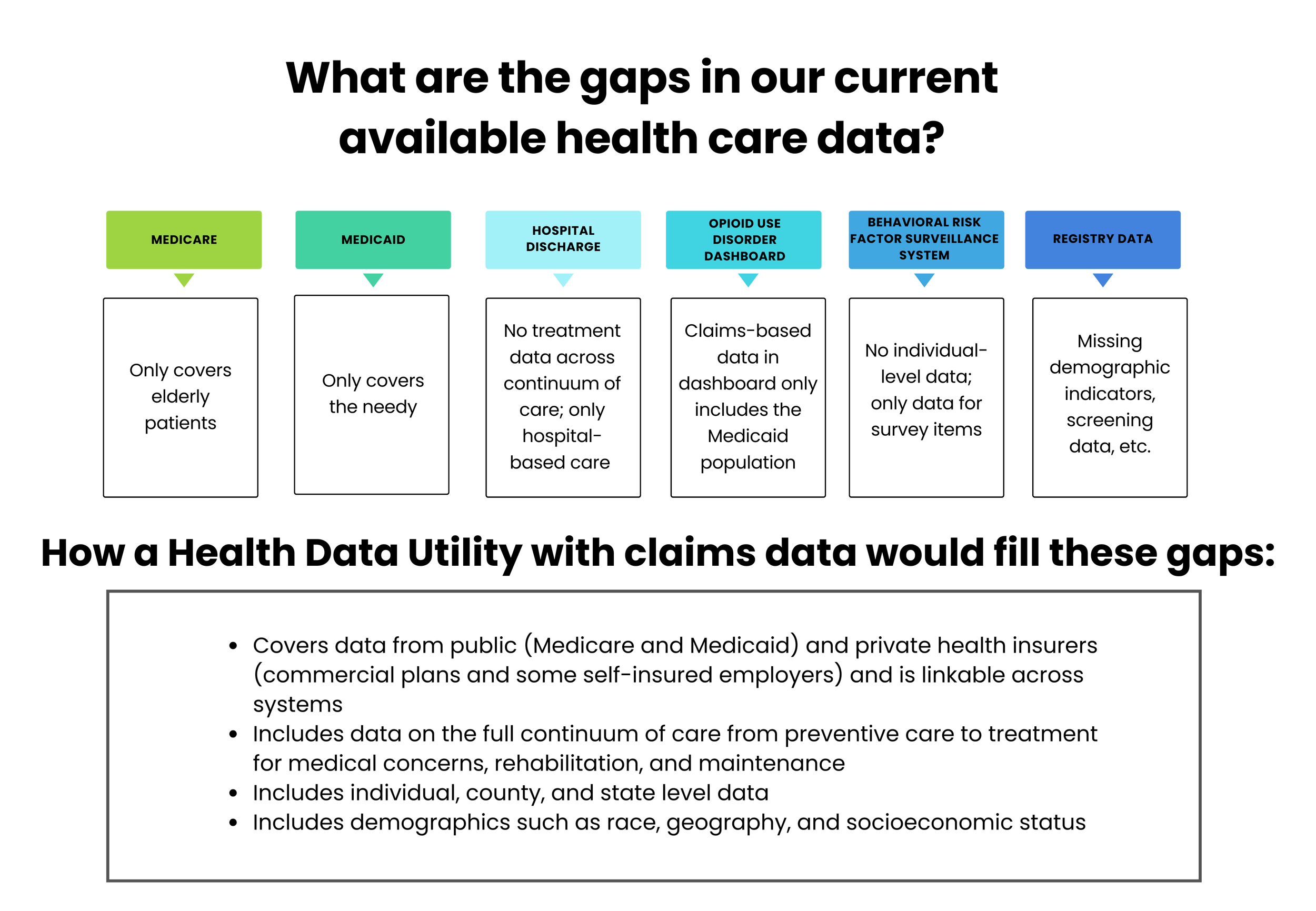
Myth number 1: We don’t need a Health Data Utility with claims data, we already have all the data available from other sources
We do have access to some data, but not in an integrated system where data is linked to provide population level analysis.
Myth number 2: Claims data is a partisan issue
Claims data is being collected in both blue and red states. See examples above.
Myth number 3: Claims data is used to regulate and cap commercial prices
Tools that gather claims data do not have the authority to regulate or cap prices. Some states (Montana, Oregon, and Washington) do cap prices, but those programs were enacted by state legislature. Claims data only provides information that can inform policymakers.
Myth number 4: Claims data violates patient privacy and put patient data at risk of a data breach
Health Data Utilities comply with Health Information Portability and Accountability Act (HIPAA) and HITECH act, National Institute of Standards and Technology (NIST), and other federal and state regulations. Data is encrypted, and submissions are sent over encrypted connections. Personal Identifiers are removed and replaced with encrypted identifiers not linked to any other source. Other identifying information is aggregated such as age, zip codes, small cell data suppression.

Data Protection
Health Data Utilities have strict safeguards and regulations in place to protect patient privacy. The data is usually anonymized before being made available for analysis, ensuring confidentiality while still allowing for valuable insights.